Modern hip replacement can look very different from what it was a few decades ago. Today’s techniques aim to relieve pain, restore movement, and help people return to their routines sooner with careful attention to safety and long-term results.
In this guide, we’ll look how conventional (standard-incision) hip replacement compares with minimally invasive approaches, what the evidence actually says about recovery and risks, who tends to benefit, how to think about costs (in INR), and how to choose an approach with your surgeon that fits your body, bone quality, and activity goals.
If you’re exploring Hip Replacement Surgery in Ahmedabad, you’ll find that both conventional and minimally invasive options are offered across India, with rehabilitation pathways that can be tailored to your lifestyle.
What happens in a hip replacement?
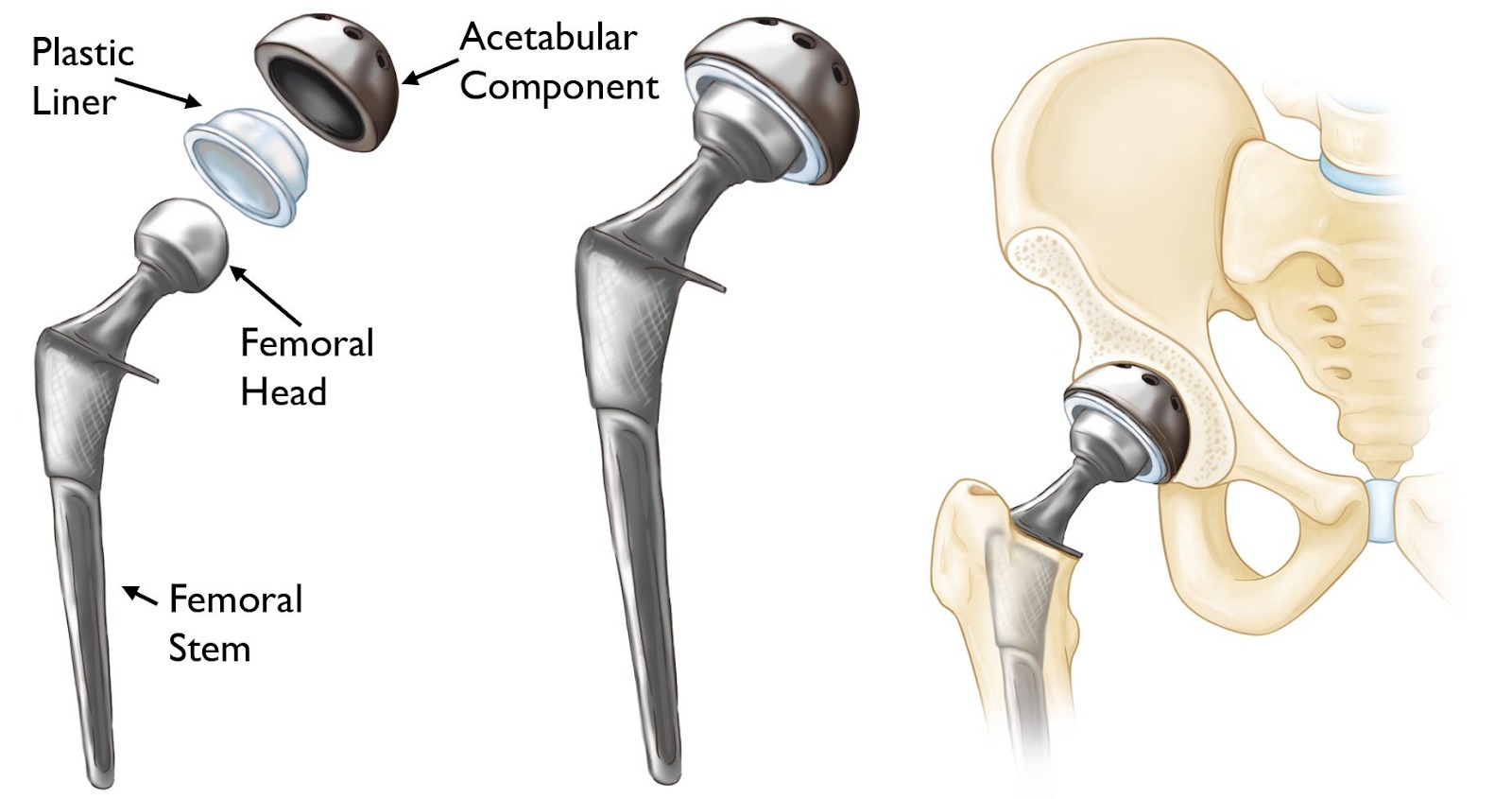
In any hip replacement, the damaged ball-and-socket joint is resurfaced with implants which is a stem fitted inside the thigh bone (femur) with a ball on top, and a cup placed in the pelvis (acetabulum).
The core difference between approaches is how the surgeon reaches the joint including the skin incision length, the muscles split or preserved, the patient’s positioning on the table, and the visualization tools the surgeon uses. These details influence early pain, walking speed, and some complication patterns, but the implant itself is not “mini” vs “standard.”
What does Minimally Invasive mean?
Minimally invasive total hip replacement typically uses a single skin incision of about 7–15 cm (roughly 3–6 inches), sometimes paired with muscle-sparing techniques; conventional approaches use longer incisions and more extensive exposure.
Exact lengths vary by body size and anatomy. Surgeons may also use two small incisions in selected cases. What matters as much as skin length is how much muscle and tendon is detached and less disruption tends to correlate with quicker early recovery.
Traditional Vs Minimally Invasive Hip Replacement Comparison
| Feature | Conventional THR | Minimally Invasive THR |
| Skin incision & exposure | Longer incision; wider exposure for a clear view of the joint | Shorter incision (often ~3–6 in / 7–15 cm); smaller window to the joint |
| Muscle/tendon handling | More soft-tissue detachment possible | Often muscle-sparing or less detachment |
| Early recovery & hospital stay | Solid outcomes but typically a bit more pain early; hospital stay can be slightly longer | Tends to have less early pain, faster first steps, and often a shorter stay |
| Implant positioning visibility | Excellent visualization; helpful in complex anatomy or deformity | Good in experienced hands, but visualization is more limited so teams may use intra-op imaging/navigation |
| Complication pattern | Lower risk of nerve irritation around the outer thigh; dislocation risk reduced with modern soft-tissue repair | Slightly higher chance of temporary outer-thigh numbness (approach-dependent); dislocation risk can be low with certain approaches |
| Who it suits best | Complex cases, very muscular builds, severe deformity/osteoporosis, or when revision is expected | Many primary (first-time) replacements with straightforward anatomy aiming for quicker early recovery |
Risks Involved in Hip Replacement Surgery
All hip replacements share certain risks:
- Infection
- Blood clots
- Dislocation
- Leg-length change
- Fracture
- Nerve or vessel injury
- Medical complications.
With smaller incisions, visualization can be more limited, which is why surgeon experience and tools (e.g., intra-op imaging, robotics, navigation) matter. Some analyses note a potential for component malposition in inexperienced hands with minimally invasive techniques. Conversely, larger exposures may include more muscle detachment, which can lengthen early recovery.
Different Treatment Approaches for Hip Replacement
Both traditional and minimally invasive surgery options have different approaches, like for instance:
Direct anterior (a common minimally invasive path): lower dislocation risk in some series, but a higher rate of temporary numbness over the outer thigh (lateral femoral cutaneous nerve irritation) can occur. Operating times may be longer during the learning curve.
Posterior or lateral (traditional exposures, now often done “mini-posterior”): wide, reliable view and excellent implant positioning in experienced hands; some data show slightly longer early hospital stays vs. mini-incision variants, though enhanced-recovery protocols are narrowing that gap.
Risk patterns differ a bit by approach, but the strongest predictor of safety is a surgeon proficient in the technique you choose.
Do Minimally Invasive Hips Last as Long?
Yes, longevity depends on the implant and bone, not the skin incision. Large registry syntheses show that about 85% of total hip replacements are still functioning at 15 years, and roughly 58% at 25 years; some case series report even higher 20–25-year survivorship with modern implants.
These figures apply to hip replacement broadly regardless of incision length because durability is driven by implant design/materials, fixation (cemented vs uncemented), surgical accuracy, and patient factors.
Who is a Good Candidate for Minimally Invasive Surgery?
Many people are candidates, including older adults, provided bone quality and anatomy are suitable. Certain situations include very muscular builds, complex deformity, severe osteoporosis, or revision surgery.
This may push a team toward a more open exposure for safety and precision. Ultimately, candidacy hinges on your imaging, bone stock, hip shape, and the surgeon’s ability to achieve stable, well-aligned implants through a smaller window.
Choosing Your Surgical Approach for Hip Replacement Surgery
It is important to be clear about which procedure might be right for you so consider these factors, for example:
1) Your anatomy and bone quality. Severe deformities, bone cysts, or very soft bone may favor a broader exposure to ensure accurate alignment and stable fixation.
2) Surgeon’s experience with the approach you prefer. Ask how many they perform annually, their dislocation and revision rates, and how they ensure accurate cup/stem positioning (fluoroscopy, navigation, robotics, intra-op x-ray). Consistency and a reproducible plan often beat chasing a trend.
3) Early recovery priorities. If your main goal is earlier walking and shorter early pain, a muscle-sparing or minimally invasive route can help, provided implant positioning is not compromised.
4) Nerve-symptom tolerance. If outer-thigh numbness would bother you, discuss the lateral femoral cutaneous nerve risk seen more often with anterior approaches and how your team mitigates it.
5) Long-term durability. Focus less on incision size and more on precision and implant choice. Modern hips commonly last 15–25 years (or longer) when well implanted and looked after.
Life after Surgery
Most people return to low-impact activity (brisk walking, cycling, swimming) over weeks to months. High-impact sports are individualized; many teams advise avoiding repetitive impact to prolong implant life. Security scanners at airports are usually fine but carry your surgical note if asked. Car travel and driving resume when you can safely brake and are off sedating pain medicines; your surgeon will give a timeline based on leg strength and reflexes.
FAQs
Is a minimally invasive hip replacement always better than a conventional one?
No. Minimally invasive surgery can speed early recovery, but long-term outcomes are comparable when implants are positioned well. The best choice is the one your surgeon can perform most accurately for your anatomy.
How long will my new hip last?
Large datasets suggest ~85% of hips last 15 years and ~58% last 25 years, with some modern series showing longer survival. Activity level, body weight, bone quality, and surgical accuracy all influence longevity.
Is the direct anterior approach riskier for nerves?
It can carry a higher chance of temporary numbness over the outer thigh (lateral femoral cutaneous nerve). Most cases improve with time; discuss your personal risk and mitigation steps with your team.
Can I sit cross-legged or on the floor after surgery?
Sometimes, but only after your surgeon clears you. It depends on your approach, implant stability, flexibility, and any precautions (some teams restrict extreme flexion and internal rotation for a period).
Will I need special implants if I’m younger and active?
Implant choice (bearing surfaces like ceramic-on-polyethylene, stem design, fixation method) is tailored to you. Younger, active patients often receive hard-wearing bearings; discuss pros and cons for wear, fracture risk, and revision ease.
How to prevent blood clots after hip replacement surgery?
Expect a prevention plan: early walking, calf pumps, and short-term blood thinners (tablets or injections) based on your personal risk profile.
Do I need to choose the approach for hip replacement or the surgeon?
Choose the surgeon and team you trust, then discuss approach options. Surgeon proficiency with a given technique is one of the strongest drivers of safe, accurate outcomes.